Fentanyl (also known as fentanil, brand names Sublimaze, Actiq, Durogesic, Duragesic, Fentora, Matrifen, Haldid, Onsolis, Instanyl, Abstral, Lazanda and others) is a potent, synthetic opioid analgesic with a rapid onset and short duration of action. It is a strong agonist at the μ-opioid receptors. Historically, it has been used to treat breakthrough pain and is commonly used in pre-procedures as a pain reliever as well as an anesthetic in combination with a benzodiazepine.
Fentanyl is approximately 80 to 100 times more potent than morphine and roughly 15 to 20 times more potent than heroin.
Fentanyl was first synthesized by Paul Janssen in 1960 following the medical inception of pethidine several years earlier. Janssen developed fentanyl by assaying analogues of the structurally related drug pethidine for opioid activity. The widespread use of fentanyl triggered the production of fentanyl citrate (the salt formed by combining fentanyl and citric acid in a 1:1 stoichiometry), which entered the clinical practice as a general anaesthetic under the trade name Sublimaze in the 1960s. Following this, many other fentanyl analogues were developed and introduced into medical practice, including sufentanil, alfentanil, remifentanil, and lofentanil.
In the mid-1990s, fentanyl was first introduced for widespread palliative use with the clinical introduction of the Duragesic patch, followed in the next decade by the introduction of the first quick-acting prescription formulations of fentanyl for personal use, the Actiq lollipop and Fentora buccal tablets. Through the delivery method of transdermal patches, as of 2012 fentanyl was the most widely used synthetic opioid in clinical practice, with several new delivery methods now available, including a sublingual spray for cancer patients. In 2013 1700 kilograms were used globally.
Fentanyl and its derivatives are used recreationally. Deaths have resulted from both recreational and improper medical use.
Medical uses
Intravenous fentanyl is often used for anesthesia and analgesia. During anaesthesia it is often used along with a hypnotic agent like propofol. Fentanyl may be included in a solution along with local anesthetic for neuraxial administration (epidural or intrathecal/spinal). It is also administered in combination with a benzodiazepine, such as midazolam, to produce procedural sedation for endoscopy, cardiac catheterization, oral surgery, etc., and is often used in the management of chronic pain including cancer pain.
In children intranasal fentanyl is useful for the treatment of moderate and severe pain and is well tolerated.
Patches
Fentanyl transdermal patch (Durogesic/Duragesic/Matrifen) is used in chronic pain management. The patches work by slowly releasing fentanyl through the skin into the bloodstream over 48 to 72 hours, allowing for long-lasting pain management. Dosage is based on the size of the patch, since, in general, the transdermal absorption rate is constant at a constant skin temperature. Rate of absorption is dependent on a number of factors. Body temperature, skin type, amount of body fat, and placement of the patch can have major effects. The different delivery systems used by different makers will also affect individual rates of absorption. Under normal circumstances, the patch will reach its full effect within 12 to 24 hours; thus, fentanyl patches are often prescribed with a fast-acting opiate (such as morphine or oxycodone) to handle breakthrough pain.
In palliative care, transdermal fentanyl has a definite, but limited, role for:
- people already stabilized on other opioids who have persistent swallowing problem and cannot tolerate other parenteral routes such as subcutaneous administration.
- people with moderate to severe renal failure.
- troublesome side effects of oral morphine, hydromorphone, or oxycodone.
Lozenges
Fentanyl lozenges (Actiq) are a solid formulation of fentanyl citrate on a stick in the form of a lollipop that dissolves slowly in the mouth for transmucosal absorption. These lozenges are intended for opioid-tolerant individuals and are effective in treating breakthrough cancer pain. It has also been used for breakthrough pain for patients with nonmalignant (not cancer related) pain, but this application is controversial. The unit is a berry-flavored lozenge on a stick swabbed on the mucosal surfaces inside the mouth â€" inside of the cheeks, under and on the tongue and gums â€" to release the fentanyl quickly into the system. It is most effective when the lozenge is consumed within 15 minutes. About 25% of the drug is absorbed through the oral mucosa, resulting in a fast onset of action, and the rest is swallowed and absorbed in the small intestine, acting more slowly. The lozenge is less effective and acts more slowly if swallowed as a whole, as despite good absorbance from the small intestine there is extensive first-pass metabolism, leading to an oral bioavailability of about 33% as opposed to 50% when used correctly (25% via the mouth mucosa and 25% via the gut).
However, most people find that it takes 10â€"15 minutes to use all of one lozenge, and those with a dry mouth cannot use this route. In addition, medical personnel are unable to document how much of a lozenge has been used by a person, making drug records inaccurate.
Other
A wide range of fentanyl preparations is available, including buccal tablets or patches, nasal sprays, inhalers, and active transdermal patches (heat or electrical). Some preparations such as nasal sprays and inhalers may result in a rapid response, but the fast onset of high blood levels may compromise safety. In addition, the expense of some of these appliances may greatly reduce their cost-effectiveness. In children it is unclear if intranasal fentanyl is as good as or same as morphine.
Fentanyl is sometimes given intrathecally as part of spinal anesthesia or epidurally for epidural anesthesia and analgesia. Because of fentanyl's high lipid solubility, its effects are more localized than morphine, and some clinicians prefer to use morphine to get a wider spread of analgesia.
Veterinary use

Fentanyl (in injectable formulation) is commonly used for analgesia and as a component of balanced sedation and general anesthesia in small animal patients. Its potency and short duration of action make it particularly useful in critically ill patients. In addition, it tends to cause less vomiting and regurgitation than do other pure-opioid agonists (morphine, hydromorphone) when given as a continuous infusion post-operatively. As with other pure opioids, fentanyl can be associated with dysphoria in both dogs and cats.
Transdermal fentanyl has also been used for many years in dogs and cats for post-operative analgesia. Most commonly this has been accomplished by off-label use of fentanyl patches manufactured for use in humans with chronic malignant pain. In 2012 a highly concentrated (50Â mg/ml) transdermal solution, trade name Recuvyra, has become commercially available for use in dogs only. It is FDA approved to provide four days of analgesia (again in dogs only) after a single application prior to surgery. It is not approved for multiple doses or use in other species. The drug is also approved in Europe.
Adverse effects

Fentanyl's most common side-effects (more than 10% of patients) include diarrhea, nausea, constipation, dry mouth, somnolence, confusion, asthenia (weakness), and sweating and, less frequently (3 to 10% of patients), abdominal pain, headache, fatigue, anorexia and weight loss, dizziness, nervousness, hallucinations, anxiety, depression, flu-like symptoms, dyspepsia (indigestion), dyspnea (shortness of breath), hypoventilation, apnea, and urinary retention. Fentanyl use has also been associated with aphasia.
Despite being a more potent analgesic, fentanyl tends to induce less nausea, as well as less histamine-mediated itching, in relation to morphine.
Fentanyl may produce more prolonged respiratory depression than other opioid analgesics. In 2006 the U.S. Food and Drug Administration (FDA) began investigating several respiratory deaths, but doctors in the United Kingdom were not warned of the risks with fentanyl until September 2008. The FDA reported in April 2012 that young children had died or become seriously ill from accidental exposure to a fentanyl skin patch.
The precise reason for sudden respiratory depression is unclear, but there are several hypotheses:
- Saturation of the body fat compartment in patients with rapid and profound body fat loss (patients with cancer, cardiac or infection-induced cachexia can lose 80% of their body fat).
- Early carbon dioxide retention causing cutaneous vasodilatation (releasing more fentanyl), together with acidosis, which reduces protein binding of fentanyl, releasing yet more fentanyl.
- Reduced sedation, losing a useful early warning sign of opioid toxicity and resulting in levels closer to respiratory-depressant levels.
Fentanyl has a therapeutic index of 270.
Storage and disposal
Fentanyl is one of a small number of drugs that may be especially harmful, and in some cases fatal, with just one dose, if used by someone other than the person for whom the drug was prescribed. All fentanyl medicine should be kept in a secure location such as a locked cabinet that is out of children’s sight and reach.
When they cannot be disposed of through a drug take-back program, flushing is recommended for fentanyl medicines because it is the fastest and surest way to remove these potent medicines from the home so they cannot harm children, pets, and others not intended to use them.
Fentanyl patches should be flushed down the toilet as soon as they are removed from the body, and unused fentanyl patches should be flushed as soon as they are no longer needed. Detailed "Instructions for Use", with complete information on how to apply, use, and dispose of fentanyl patches, are available on the FDA website.
Overdoses and fatalities
In 2009, the former guitarist for the band Wilco, Jay Bennett, died in his sleep of an overdose of the drug via Duragesic time-release patches prescribed for him. In 2010, band Slipknot's bassist Paul Gray overdosed and died after using a mixture of fentanyl and morphine, for which there was no evidence of a prescription. An inquest jury found by a majority verdict of 3-2 that an overdose of fentanyl was responsible for the death by misadventure of Anita Chan Lai-ling, 69, who died on October 17, 2007, after she was given an overdose of fentanyl. On June 27, 2005, Laurence Harvey's daughter Domino Harvey was found unconscious in her bathtub, and the Los Angeles County Coroner's office determined that she had overdosed on fentanyl. In 2009 27-year-old Hayley Fisher, a midwife at King Edward Memorial Hospital for Women in Australia, died after injecting herself with fentanyl.
In July 2014, the Medicines and Healthcare Products Regulatory Agency (MHRA) issued a warning about the potential for life-threatening harm from accidental exposure to transdermal fentanyl patches, particularly in children, and advised that they should be folded, with the adhesive side in, before being discarded. The patches should be kept away from children, who are most at risk from fentanyl overdose.
Analogues
Structural analogs of fentanyl include:
- Alfentanil (trade name Alfenta), an ultra-short-acting (five- to 10-minute) analgesic.
- Sufentanil (trade name Sufenta), a potent analgesic (five to 10 times more potent than fentanyl) for use in specific surgeries and surgery in heavily opioid-tolerant/opioid-dependent patients. Its binding affinity is high enough to theoretically break through a buprenorphine blockade to offer pain relief from acute trauma in patients taking high-dose buprenorphine.
- Remifentanil (trade name Ultiva), currently the shortest-acting opioid, has the benefit of rapid offset, even after prolonged infusions.
- Carfentanil (trade name Wildnil) is an analogue of fentanyl with an analgesic potency 10,000 times that of morphine and is used in veterinary practice to immobilize certain large animals such as elephants.
- Lofentanil is an analogue of fentanyl with a potency slightly greater than that of carfentanil.
- 3-Methylfentanyl (thought to be the active constituent of Kolokol-1, a chemical weapon)
- 3-Methylthiofentanyl
- Acetyl-α-methylfentanyl
- α-Methylfentanyl (see below)
- α-Methylthiofentanyl
- β-Hydroxy-3-methylfentanyl
- β-Hydroxyfentanyl
- p-Flurorofentanyl
- Thiofentanyl
- Acetylfentanyl
- Butyrfentanyl
- Furanyl-fentanyl
- The tropane analog of fentanyl was prepared (2 isomers).
- Acryloyl analog of fentanyl 2x potency/duration of regular fentanyl (Egyptian scientist).
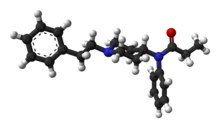
Mechanism of action
Fentanyl provides some of the effects typical of other opioids through its agonism of the opioid receptors. Its strong potency in relation to that of morphine is largely due to its high lipophilicity, per the Meyer-Overton correlation. Because of this, it can more easily penetrate the CNS.
History
Fentanyl was first synthesized by Paul Janssen under the label of his relatively newly formed Janssen Pharmaceutica in 1959. In the 1960s, fentanyl was introduced as an intravenous anesthetic under the trade name of Sublimaze. In the mid-1990s, Janssen Pharmaceutica developed and introduced into clinical trials the Duragesic patch, which is a formation of an inert alcohol gel infused with select fentanyl doses, which are worn to provide constant administration of the opioid over a period of 48 to 72Â hours. After a set of successful clinical trials, Duragesic fentanyl patches were introduced into the medical practice.
Following the patch, a flavored lollipop of fentanyl citrate mixed with inert fillers was introduced under the brand name of Actiq, becoming the first quick-acting formation of fentanyl for use with chronic breakthrough pain. More recently, fentanyl has been developed into an effervescent tab for buccal absorption much like the Actiq lollipop, followed by a buccal spray device for fast-acting relief and other delivery methods currently in development.
A fentanyl product has been approved by the US Food and Drug Administration (FDA) for breakthrough cancer pain called Onsolis. It uses a drug delivery technology called BEMA (fentanyl buccal soluble film) on a small disc placed in the mouth. Unlike many other fentanyl products, the drug cannot be abused by crushing and inhaling.
Fentanyl has a US DEA ACSCN of 9801 and a 2013 annual aggregate manufacturing quota of 2108.75 kilos, unchanged from the prior year.
Recreational use
Illicit use of pharmaceutical fentanyl and its analogues first appeared in the mid-1970s in the medical community and continues in the present. United States authorities classify fentanyl as a narcotic and an opioid. To date, more than 12 different analogues of fentanyl have been produced clandestinely and identified in the U.S. drug traffic. The biological effects of the fentanyl analogues are similar to those of heroin, with the exception that many users report a noticeably less euphoric "high" associated with the drug and stronger sedative and analgesic effects.
Fentanyl analogues may be hundreds of times more potent than street heroin, and tends to produce significantly more respiratory depression, making it somewhat more dangerous than heroin to users. Fentanyl is used orally, smoked, snorted, or injected. Fentanyl is sometimes sold as heroin, often leading to overdoses. Many fentanyl overdoses are initially classified as heroin overdoses. In Estonia, due to its high rate of recreational use, fentanyl causes more deaths nationwide than traffic accidents.
Fentanyl is sometimes sold on the black market in the form of transdermal fentanyl patches such as Duragesic, diverted from legitimate medical supplies. The patches may be cut up and eaten, or the gel from inside the patch smoked.
Another dosage form of fentanyl that has appeared on the streets is the Actiq fentanyl lollipops, which are sold under the street name of "percopop". The pharmacy retail price ranges from US$15 to US$50 per unit (based on strength of lozenge), with the black market cost anywhere from US$20 to US$80 per unit, depending on the strength.
Non-medical use of fentanyl by individuals without opiate tolerance can be very dangerous and has resulted in numerous deaths. Even those with opiate tolerances are at high risk for overdoses. Once the fentanyl is in the user's system, it is extremely difficult to stop its course because of the nature of absorption. Illicitly synthesized fentanyl powder has also appeared on the United States market. Because of the extremely high strength of pure fentanyl powder, it is very difficult to dilute appropriately, and often the resulting mixture may be far too strong and, therefore, very dangerous.
Some heroin dealers mix fentanyl powder with heroin to increase potency or compensate for low-quality heroin. In 2006, illegally manufactured, non-pharmaceutical fentanyl often mixed with cocaine or heroin caused an outbreak of overdose deaths in the United States, heavily concentrated in the cities of Dayton, (Ohio), Chicago, Detroit, and Philadelphia, as well as Baltimore, Pittsburgh, St. Louis, Milwaukee, and Camden (New Jersey). Little Rock and Dallas were also affected. The mixture of fentanyl and heroin is known as "magic" or "the bomb", among other names, on the street.
Several large quantities of illicitly produced fentanyl have been seized by U.S. law enforcement agencies. In June 2006, 945Â grams of 83%-pure fentanyl powder was seized by Border Patrol agents in California from a vehicle that had entered from Mexico. Mexico is the source of much of the illicit fentanyl for sale in the U.S. However, in April 2006, there was one domestic fentanyl lab discovered by law enforcement in Azusa, California. The lab was a source of counterfeit 80-mg OxyContin tablets containing fentanyl instead of oxycodone, as well as bulk fentanyl and other drugs.
The "China White" form of fentanyl refers to any of a number of clandestinely produced analogues, especially α-methylfentanyl (AMF). This Department of Justice document lists "China White" as a synonym for a number of fentanyl analogues, including 3-methylfentanyl and α-methylfentanyl, which today are classified as Schedule I drugs in the United States. Part of the motivation for AMF is that, despite the extra difficulty from a synthetic standpoint, the resultant drug is relatively more resistant to metabolic degradation. This results in a drug with an increased duration.
In June 2013, the United States' Centers for Disease Control and Prevention (CDC) issued a health advisory to emergency departments alerting to 14 overdose deaths among intravenous drug users in Rhode Island associated with acetylfentanyl, a novel, injected, non-prescription synthetic opioid analog of fentanyl.
Military use
Analgesic
The Danish Army uses the fentanyl stick in military operations as a painkiller. The war documentary Armadillo (2010) features an interview with a Danish medic who tells of using fentanyl on a severely wounded soldier in Afghanistan.
The United States Air Force Pararescue and Swedish armed forces combat medics utilize lollipops with fentanyl.
As a poison
It is alleged that Mossad agents used "levofentanyl" in their 1997 attempt to kill Hamas leader Khalid Mishal. However, since fentanyl is achiral (i.e., has no "levo-" form), the substance was probably fentanyl itself, a fentanyl analogue, or another opioid. However, it could have been a non-opioid sedative or unknown drug.
See also
- 3-Methylbutyrfentanyl
- 3-Methylfentanyl
- 4-Fluorofentanyl
- α-Methylfentanyl
- Acetylfentanyl
- Butyrfentanyl
- Furanylfentanyl
- List of Fentanyl analogues
References
External links
- National Institute of Health (NIH) Medline Plus: Fentanyl Buccal (Transmucosal)
- RxList: Fentanyl
- US DEA information: fentanyl
- 08/16/2007 News Release: Cephalon Announces Positive Results from a Pivotal Study of FENTORA in Opioid-tolerant Patients with Non-cancer Breakthrough Pain
- BBC news report on Russian siege story
- Fentanyl: Emergency Response Database. National Institute for Occupational Safety and Health.
- U.S. National Library of Medicine: Drug Information Portal - Fentanyl
